If your child is anxious. Or angry. Or just seems lost in ways you can’t quite name. Someone has probably mentioned behavioral therapy. A doctor. A counselor. Maybe a friend in the school pickup line. The words land heavy. You don’t know exactly what it means. You only know it keeps coming up, and you’re left wondering if this is something that could actually help.
Kids learn by doing. Tying shoes. Riding bikes. Copying the little phrases they hear at home. They also learn the less helpful things. Shutting down. Avoiding. Exploding over something small. Behavioral therapy is focused on changing maladaptive behaviors through reinforcement and behavioral therapy techniques rooted in learning. If children can learn patterns that don’t work, they can also learn new behaviors.
It isn’t just talk therapy about feelings. That rarely sticks with kids. A good mental health professional acts more like a coach. They teach skills. They practice skills in real time, using behavior therapy techniques like reinforcement, modeling, and exposure. When anger spikes, here’s what to do. When fear shows up, here’s how to stay with it instead of running. When thoughts spiral, here’s how to catch them.
Unlike vague discussions, this therapy is pointed. If your child fears dogs, sessions use systematic desensitization and exposure therapy, starting small and building tolerance. If your child struggles with anger, sessions target problematic behaviors directly.
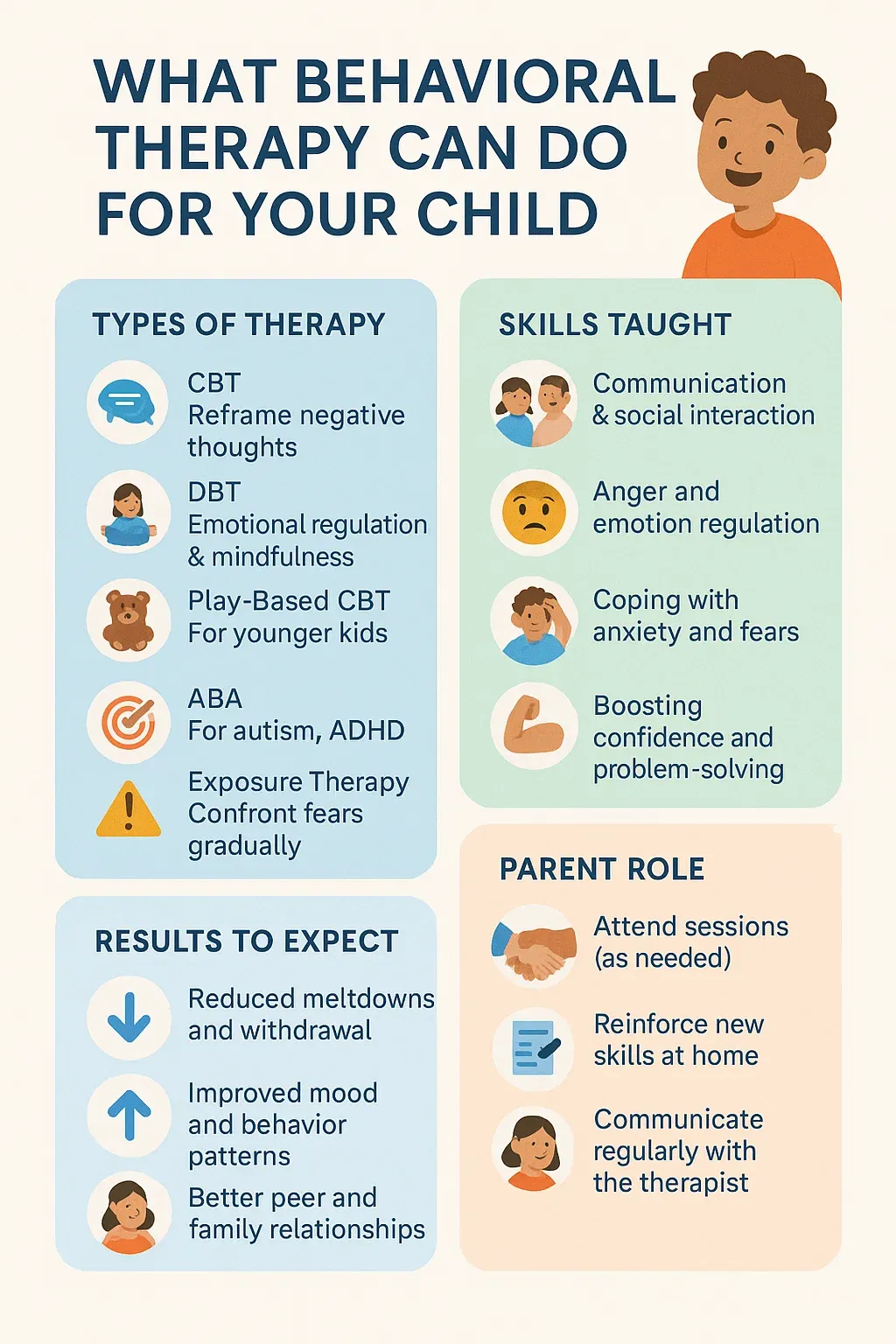
There isn’t just one version—there are several behavioral approaches:
Cognitive Behavioral Therapy (CBT): A structured, goal-oriented form of psychological therapy that combines cognitive therapy (thought patterns) with behavior therapy (action patterns). It helps kids notice problematic thoughts like “nobody likes me,” question them, and replace them. About 75% of people who enter CBT experience some benefits, and it’s considered the gold standard for treating mental health conditions like anxiety disorders, depression, and post traumatic stress disorder.
Dialectical Behavior Therapy (DBT): Best for children who feel emotions intensely. It uses mindfulness, coping skills, and commitment therapy strategies to manage overwhelming feelings and reduce suicidal behavior or impulsive outbursts. Cognitive Behavioral Play Therapy: For younger kids, therapists blend play with cognitive behavioural therapy, using toys and games to build coping skills and reduce emotional challenges.
Applied Behaviour Analysis and behavioral classroom management: These approaches are often used with children with autism or ADHD, reinforcing desirable behaviors and discouraging maladaptive behaviors through operant conditioning and positive reinforcement.
Aversion therapy: Pairs a negative stimulus with an unwanted action, discouraging problematic behaviors like substance misuse.
Behavioral activation: Encourages depressed kids to re-engage in rewarding activities, preventing withdrawal. Each uses reinforcement to encourage desirable behaviors while teaching children healthier patterns.
The basic principles are straightforward. Reinforcement shows kids that effort brings rewards. Therapists might reinforce desirable behaviors with praise, privileges, or other rewards. Systematic desensitization teaches children to face fears step by step while practicing stress management and relaxation techniques.
Sessions also tackle problematic thoughts. Kids learn to test whether extreme fears are realistic, using cognitive interventions. For depression, therapists encourage activities (sports, drawing, seeing friends) to break avoidance cycles. Behavioral activation can gradually lift mood.
Therapists also teach relaxation skills—deep breathing, progressive muscle relaxation, guided imagery. These taught skills give children coping skills to handle emotional challenges in the moment.
Behavioral and cognitive therapies have wide applications. They are effective in treating mental health conditions such as:
It can also support kids with autism spectrum disorder and ADHD by teaching social skills and reducing problematic behaviors. Studies show approximately 67% of people who try psychotherapy experience improvement with behavioral therapy techniques. Research also shows that behavioral interventions enhance health outcomes in chronic pain and chronic disease management.
A typical therapy session runs 45–60 minutes. At first, it’s about trust. Then, sessions follow a rhythm: check in, practice a skill, discuss outside progress. Homework often reinforces new behaviors at home.
Sessions may include commitment therapy exercises based on relational frame theory—helping kids accept feelings without letting them control actions. Over time, functional assessments and treatment plans are adjusted as the child progresses.
Behavioral therapy requires collaboration from parents, teachers, and sometimes peers. Through behavioral parent training, therapists teach parents how to reinforce desirable behaviors at home. Behavioral peer interventions also help children through modeling and encouragement from classmates. Parents are part of the team, reinforcing skills, watching for problematic behaviors, and supporting treatment plans. This collaboration often leads to positive social interactions and stronger interpersonal relationships.
Finding the right mental health professional can feel overwhelming. Start with your pediatrician or healthcare professionals you trust. Social workers and psychologists can also recommend options. Check credentials—ensure your provider has the right certifications in behavior therapy or cognitive behavioral therapy. Most health insurance plans cover therapy for mental health problems. Don’t hesitate to meet several therapists; you’ll know the right fit when you feel comfortable.
Behavioral therapy doesn’t erase problems overnight, but it provides several core principles and tools to create positive behavioral patterns. With structured treatment plans, reinforcement, and behavioral therapy techniques, children learn desirable behaviors that improve both their emotional health and physical well being. Whether it’s cognitive behavioral therapy, dialectical behavior therapy, or other forms of structured care, these behavioral approaches help kids face fears, reduce severe symptoms, and build resilience. And while it may feel daunting, choosing therapy is an act of care—a way to help your child gain insight, practice taught skills, and build confidence for everyday life.
Our team of experienced therapists is dedicated to helping children with autism and other developmental disabilities reach their full potential. We are committed to creating a supportive and nurturing environment where every child can thrive.
Contact us today to learn more about our services and how we can support your child's development.